 Image courtesy of the National Institutes of Health
Image courtesy of the National Institutes of Health
By Cat Troiano
According to the American Liver Foundation, nearly 30,000 adults are diagnosed with liver cancer each year, and the number of mortalities exceeds 20,000 annually. Additional diseases threaten the liver, including some that can be just as deadly and some that can be prevented. Evaluating liver function is a key first step toward detecting liver disease at an early stage.
Liver at Large
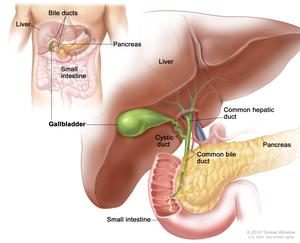
Weighing in at roughly three pounds, the liver, which is situated on the right side of the abdomen, is one of the largest organs of the human body, ranking as the second-largest organ after skin. The liver is unique in that when it sustains damage, it has the ability to regenerate as long as at least 25 percent of its tissue remains healthy. Technically a gland that is classified as part of the digestive system, the liver carries a lot of responsibilities. Functions of the liver include:
• The liver produces bile, a substance that aids in digestion and is made up of bilirubin, electrolytes, cholesterol and water.
• The liver produces albumin, which is a protein found in blood serum.
• The liver breaks down and metabolizes proteins.
• The bile that is produced in the liver metabolizes fats.
• The liver metabolizes carbohydrates to maintain blood glucose levels.
• The liver stores carbohydrates as glycogen, which can be called on by the body for use when a burst of energy is needed.
• The liver also stores a supply of vitamins, including A, B12, D, E and K.
• The liver also stores ferritin, a form of iron that comes from hemoglobin and is utilized in the production of new red blood cells.
• The liver filters hormones as well as foreign substances, such as drugs and alcohol, from the blood.
• The liver plays a role in the body’s immune function.
With so many vital roles that affect overall health, monitoring the liver’s ability to carry out these tasks efficiently is an important step in diagnosing diseases that can hinder liver function.
Diseases of the Liver
There are several diseases that affect the liver. Some examples of liver diseases include:
• Cirrhosis – a disease in which scar tissue overtakes healthy liver tissue. This process, called fibrosis, has a number of causes, including excessive alcohol use, toxins and hepatitis. Alcoholic liver disease is the leading worldwide cause of cirrhosis of the liver.
• Hepatitis – a liver infection in which the liver becomes inflamed. Viruses, toxins and autoimmune response can cause hepatitis.
• Fatty liver disease – a condition in which fat accumulates in the liver’s cells. While alcoholism is a frequent culprit, obesity can also result in fatty liver disease.
• Primary sclerosing cholangitis (PSC) – an incurable disease characterized by inflammation of the bile ducts. The cause of PSC remains unknown.
• Gilbert’s syndrome – a non-threatening condition in which bilirubin is not fully broken down, resulting in mild jaundice.
• Fascioliasis – a parasitic infection that is caused by liver flukes.
• Liver cancer – the sixth most commonly diagnosed form of cancer
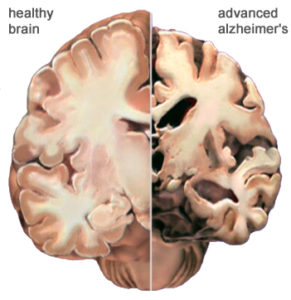
Symptoms of liver disease include jaundice, light-colored stools, dark-colored urine, appetite loss, nausea, diarrhea, fatigue, unexplained changes in weight and abdominal swelling or discomfort, but the liver may sustain extensive damage before symptoms present. Early detection through routine laboratory screening is valuable so that treatment protocols can be initiated to restore the liver’s form and function when possible.
Liver Tests and Values
A comprehensive metabolic profile is an effective routine laboratory test for analyzing a patient’s liver function. There are six results on a comprehensive metabolic profile that represent liver function.
Alanine amino transferase (ALT, or SGPT) is an enzyme that aids in metabolizing protein and converting food into energy molecules. ALT is found primarily in a healthy liver, with only low levels detected in the blood. When the liver sustains damage, however, the damaged cells release ALT into the bloodstream. An abnormally high level of ALT in the blood is indicative of liver disease.
Aspartate amino transferase (AST, or SGOT) is an enzyme that metabolizes the amino acid alanine. AST is normally found in the liver, as well as in the heart and muscles. When the liver, heart or muscles sustain damage, elevated amounts of AST are released into the bloodstream. While a high ALT level is evidence of liver disease, a normal ALT level combined with a high AST level can be indicative of a heart condition or muscle damage.
Alkaline phosphatase (ALP) is an enzyme that is found in the liver, bile ducts and bone. Damage to any of these structures causes an elevation in the ALP level in the bloodstream. High ALP levels may indicate liver disease, a bile duct obstruction or a bone disease.
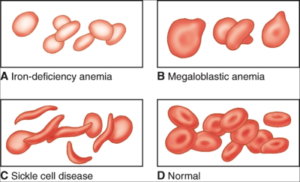
Bilirubin is a waste product that is produced when red blood cells break down at the end of their typical 120-day lifespan. Bilirubin then circulates through the liver, where it is filtered from the blood to exit the body through stool. Liver damage or disease as well as certain types of anemia can result in an elevated bilirubin level. Jaundice is a visible sign in a patient who has a very high bilirubin level.
Albumin is a protein that is produced in the liver, and it accounts for roughly 60 percent of total protein found in the blood. Albumin is essential for nourishing the body’s tissues as it aids in transporting vitamins, minerals and hormones throughout the body. When the liver is damaged, a low albumin level in the blood results.
Total protein, or albumin/globulin(A/G) ratio, represents the combined total of albumin and globulin, which accounts for the remaining 40 percent of protein that is found in the blood. Proteins are the building blocks for all cells and tissues through the body. In a patient with severe liver disease, the level of either albumin or globulin is low.
The normal ranges for liver values are:
ALT: 7 to 55 U/L
ALP: 45 to 115 U/L
AST: 8 to 48 U/L
Bilirubin: 0.1 to 1.2 mg/dL
Albumin: 3.5 to 5.0 g/dL
Total Protein: 6.3 to 7.9 f/dL
Other Liver Function Tests
When any of the aforementioned liver function values yield abnormal results on the comprehensive metabolic profile, additional tests may be ordered to aid in diagnosis. Such laboratory tests include:
Gamma-glutamyl transferase (GGT) is an enzyme that is present in the highest concentrations within the liver. While GGT levels increase as a result of liver damage incurred by any of the liver diseases, it is the first liver enzyme to become elevated when bile duct obstruction occurs. Therefore, the GGT test is useful in determining if an elevated ALP level is due to a blocked bile duct. It can also help to rule out bone disease as a cause of the elevated ALP level.
The normal reference range for GGT is 9 to 48 U/L.
Lactate dehydrogenase (LD, or LDH) is an enzyme that is found in nearly all cells throughout the body. Its highest concentrations are found in those of the liver, kidneys, heart, muscles and lungs, making the result of this test nonspecific when performed alone. When an LD is performed to compare the result against those of the comprehensive metabolic profile, it can be helpful in pinpointing the organ that has sustained tissue damage. A high LD is indicative of tissue damage.
The normal reference range for LD is 122 to 222 U/L.
Prothrombin time (PT) is a measurement of how long the blood takes to clot. Prothrombin is a protein that aids in blood coagulation. Since prothrombin is produced in the liver, the level of prothrombin that is produced can decrease if the liver is damaged or diseased, resulting in a longer blood clotting time.
The normal reference range for patients who are not taking blood thinning medications is 9.5 to 13.8 seconds.
Alpha-feto protein (AFP) is a protein that results when liver cells regenerate. Chronic liver diseases can result in ongoing elevated AFP levels in the blood. The AFP test is also a valuable tumor marker test in that very high levels of AFP are indicative of hepatocellular carcinoma and hepatoblastoma, which are two forms of liver cancer.
The normal reference range for AFP is 0 to 15 IU/ml.
Additional specific laboratory tests, such as the acute hepatitis panel and the autoimmune antibody test, can be ordered to screen for hepatitis A, B and C or autoimmune hepatitis. Diagnostic imaging tests, such as ultrasound or CT scan, may be ordered to visually reveal liver damage, structural abnormalities or masses. A liver biopsy and tissue pathology may be ordered when liver cancer is suspected.
Who Should Be Tested?
While a comprehensive metabolic panel is typically ordered as part of a routine health examination, physicians should also order the screening and/or additional liver tests in patients who are at risk for liver disease. Such situations include:
• Patients who present with the aforementioned symptoms of liver disease
• Patients who are alcoholics
• Patients with family histories of liver disease
• Patients who are overweight or obese
• Patients who may have been exposed to any of the hepatitis viruses
Some herbal remedies and a number of medications, including acetaminophen, non-steroidal anti-inflammatory drugs, statins, hormonal drugs, some antibiotic drugs and antihypertensive drugs as well as certain medications used to treat gastroesophageal reflux, diabetes, gout, allergies, fungal infections, cancer and seizures, can have adverse effects on the liver. Patients who take any such medications should be tested periodically to monitor liver health.
Treatment for liver disease depends on the specific condition that is diagnosed. Some forms of liver disease can be treated with changes in lifestyle habits, such as losing weight or ceasing alcohol consumption, while more severe forms of liver disease may progress to the point of requiring a liver transplant. Adopting healthy lifestyle habits and undergoing periodic routine laboratory tests the enable early detection offer patients the best chance for preserving liver function.