We are here for all your Physician Office Laboratory needs!



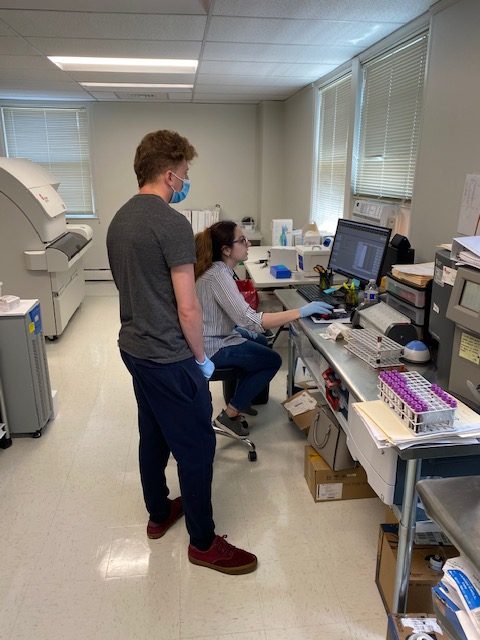
Pictured above from left: Larry Fox, Lab Director, Maya Cohen and Gina DeLisa, Lab Technologists, and Cormac Barrett, VP of Lab Sales.
By Larry Fox
We are here for all your Physician Office Laboratory needs!



Pictured above from left: Larry Fox, Lab Director, Maya Cohen and Gina DeLisa, Lab Technologists, and Cormac Barrett, VP of Lab Sales.
By Larry Fox
As we enter Phase 2 of reopening, we begin to train our team to assist Lab Techs in Lab procedures and equipment.

By Larry Fox
By Cat Troiano
From health headlines featuring Steve Jobs, Patrick Swayze, Aretha Franklin and Alex Trebek to what seems like monthly promotions for the Lustgarten Foundation and its sponsored pancreatic cancer research fundraising events, fears of pancreatic cancer have become commonplace, especially when one experiences any of the generalized symptoms. While it is the fourth leading cause of cancer death and makes up roughly seven percent of all diagnosed cancer cases, it is important to remember that the pancreas has multiple functions and that dysfunction can be the result of any of several other conditions, many of which can be successfully managed when pancreatic values are routinely assessed.
The pancreas is a gland that aids in digestion and is situated horizontally across the dorsal side of the abdominal cavity behind the stomach and inferior to the liver. The wider head of this roughly six-inch long gland can be found on the right side, connecting to the duodenum via the pancreatic duct, and the narrower tail end can be found alongside the spleen on the left side of the abdomen.
There are two main functions of the pancreas. One, the exocrine function, produces digestive enzymes which are secreted into the small intestine to continue breaking down partially digested food that has exited the stomach. These enzymes and the macronutrients that they break down are:
The bile duct, through which bile moves from the liver and gallbladder into the small intestine, runs through the pancreas and merges with the pancreatic duct at the opening to the duodenum, which is the first section of the small intestine.
The second function, the endocrine function, aids in the regulation of the body’s blood glucose level. The cell clusters that perform this function are the islets of Langerhans. These cells can be further divided into alpha cells and beta cells, each with their own role in keeping blood glucose levels within normal parameters.
Insulin transports glucose from the bloodstream to the body’s tissues to supply energy. Excess glucose is moved via insulin to the liver, where it is stored as glycogen, which can be converted into glucose when the body requires more energy, such as when exercising. Insulin also promotes the uptake of fats and amino acids into cells for storage.
Failure of the pancreas to produce and maintain proper levels of enzymes and/or hormones can result in a number of conditions that can ultimately affect other systems in the body.
There are a number of conditions that affect the pancreas.
Pancreatitis: one of the most common conditions is pancreatitis, which is an inflammation of the pancreas in which the pancreas’ own enzymes, in essence, start to digest the pancreas. Pancreatitis may be chronic or, much less commonly, acute. Excessive alcohol consumption and gallstones are all contributors to this painful condition. The longer the inflammation continues, the more damage the pancreas may sustain, which can lead to secondary conditions, such as diabetes. Hereditary pancreatitis is a genetic condition in which an individual has inherited a problem with his or her pancreas which causes him or her to experience repeated bouts of pancreatitis.
Pancreatic cancer: this form of cancer is the fourth and fifth most frequently diagnosed cancer in men and women, respectively, within the United States, and its poor prognosis makes it one of the most dreaded cancers. Potential risk factors for the development of pancreatic cancer include smoking, excessive alcohol consumption, chronic pancreatitis, liver disease and diabetes.
Type 1 diabetes: typically diagnosed early in life, this form of diabetes is essentially an autoimmune disorder in which the body’s immune system destroys the pancreas’ beta cells, rendering the pancreas unable to produce insulin.
Type 2 diabetes: this form of diabetes, which is the most prevalent form of diabetes, is a chronic metabolic disease in which the body’s tissues are unable to utilize insulin efficiently to maintain normal blood glucose levels.
Cystic fibrosis: this recessive genetic condition can affect multiple organ systems, including the pancreas. Cystic fibrosis results in the production of thick mucus that can block the pancreatic duct, preventing the release of enzymes and thus inhibiting digestion.
Exocrine pancreatic insufficiency: this is a condition in which the pancreas fails to produce or move adequate levels of enzymes for proper digestion in the intestine. Exocrine pancreatic insufficiency can result from repeated bouts of pancreatitis.
Pancreatic cysts: cysts can develop on the pancreas. A pancreatic pseudocyst is a fluid-filled sac that can develop following a bout of pancreatitis. These pseudocysts may resolve on their own, but surgical drainage may be necessary. Any cysts must be investigated, and surgical biopsy and histopathology may be may be ordered to rule out cancer.
Zollinger-Ellison syndrome: this condition is caused by the formation of a gastinoma tumor in the pancreas or the duodenum. This tumor prompts the stomach cells to release abnormally high levels of acid.
Islet cell tumor: these tumors, which affect the endocrine portion of the pancreas and include insulinomas and glucagonomas, may be benign or malignant. These tumors produce high levels of insulin or glucagon, which are then released into the bloodstream.
A routine complete metabolic panel reveals the values for lipase, amylase and glucose, the results of which provide insight to a patient’s pancreatic health and function. Separate tests that evaluate lipase, amylase and blood glucose may also be ordered to diagnose and monitor suspected cases of pancreatic conditions, diabetes, celiac disease, Crohn disease and cystic fibrosis. Patients who present with symptoms of a pancreatic condition, such as severe upper abdominal pain, nausea, vomiting, inappetence, jaundice and fever, should undergo testing for lipase and amylase levels.
As mentioned above, lipase is responsible for breaking down fats in food, converting them into fatty acids. Fats are the most energy-dense of the three macronutrients. When the pancreas is healthy and functioning normally, the amount of lipase in the blood is typically low. If the pancreas is inflamed or diseased, damage to some of the pancreatic cells are sustained, and this leads to higher amounts of lipase that end up in the bloodstream.
The normal reference range for lipase is 0 to 160 U/L.
Conditions that can cause elevation of lipase in the blood include:
Conditions that can cause an abnormally low level of lipase in the blood include chronic pancreatic conditions that result in permanent sustained damage to the lipase-producing cells.
Amylase, also known as alpha-amylase, is responsible for breaking down carbohydrates in food, converting them into sugars. This is the body’s preferred energy source.
The normal reference range for amylase is less 23 to 85 U/L.
Conditions that can cause an elevation of amylase in the blood include, but are not limited to, the following:
Conditions that can cause abnormally low levels of amylase in the blood include:
Note that some medications can cause an elevation of amylase in the blood, including:
Amylase levels that are elevated are indicative that a problem may be present, but not necessarily one of the pancreas. Lipase levels are more specific to pancreatic function. Note that elevations of either enzyme that are three times greater than the normal reference range are characteristic of pancreatitis.
Abnormally high or low blood glucose levels can reveal how efficiently the endocrine portion of the pancreas is functioning.
– The normal reference range for a fasting blood glucose level is less than 100 mg/dL.
– A result of 100 to 125 mg/dL on a fasting blood glucose level test is indicative of prediabetes. – – When two consecutive fasting blood glucose level tests both yield results of 126 mg/dL or greater, then a diagnosis of diabetes is confirmed.
– A result of 200 or greater on a random, non-fasting blood glucose level test is also indicative of diabetes.
Read here for additional information on diabetes and diabetic testing.
A fecal chymotrypsin level test should be ordered when a patient presents with signs and symptoms of pancreatic insufficiency. Such indications include unexplained weight loss or, in children, inability to gain weight, abdominal cramping, diarrhea and foul-smelling or greasy stools.
A normal test result for someone with a healthy pancreas is a positive result, indicating the presence of chymotrypsin in the stool. A negative result indicates that the patient may have pancreatic insufficiency.
Various diagnostic imaging tests can visualize the pancreas to evaluate for any structural abnormalities that may be causing symptoms. Such tests include:
As stated above, some pancreatic conditions can lead to permanent damage to the pancreas, resulting in serious consequences. Furthermore, with most cases of pancreatic cancer, by the time symptoms present, the disease is already advanced and the prognosis is grave. Evaluating pancreatic values with routine periodic metabolic profile panels is an important key in monitoring pancreatic health and function, to catch conditions early and to thus increase the chance of halting further damage.
By Larry Fox
By Cat Troiano
Although the rate of breast cancer diagnosis has decreased over the last two decades, it is estimated that more than 300,000 women will be diagnosed with breast cancer in 2019, with more than two-thirds of these cases being invasive breast cancer. While skin cancer is the most frequently diagnosed form of cancer in women, breast cancer comes in second. When it comes to cancer-related deaths, breast cancer also comes in second, with lung cancer being the number one cause of cancer-related death in women. The projected mortality rate for women with breast cancer in 2019 is nearly 42,000. For all women and for anyone with a mother, wife, daughter or sister, these numbers are alarming. However, the mortality rate has been declining over the last 30 years, thanks in part to heightened awareness and early detection.
One of the first keys in early detection is awareness of the risk factors of breast cancer. The chances of developing breast cancer increase for individuals with the following risk factors:
Age. Women over the age of 55 account for two out of three breast cancer diagnoses, indicating that advancing age comes into play as a risk factor.
Family history. A woman’s chance of developing breast cancer doubles when a first-degree female relative, such as her mother, sister or daughter, is diagnosed.
Ethnicity. African-American women have a higher risk of developing aggressive forms of breast cancer and are typically diagnosed at a younger age. Overall, however, white women are at a slightly higher risk than African-American women for developing breast cancer, while Asian and Hispanic women have a lower risk.
Reproductive health history. Women who began menstruating prior to the age of 12 have a higher risk of developing breast cancer, as do those who go through menopause after the age of 55 and those who either never gave birth or who gave birth to their first child after the age of 30.
Prior breast cancer history. Women who have been previously diagnosed and treated for breast cancer are three to four times more likely to develop another form of breast cancer.
Prior radiation treatment. Women who receive radiation to treat a condition in the upper body, such as non-Hodgkin’s lymphoma or Hodgkin’s disease, at less than 30 years of age are at increased risk for developing breast cancer.
Breast composition. Women with non-cancerous, or benign, beast conditions as well as those with dense breast tissue have higher risks for developing breast cancer.
Chemical exposure. Women who are frequently exposed to certain chemical substances found in food, cosmetics, skin care products, lawn and gardening chemicals, plastics and even water have higher risks of developing breast cancer.
Lifestyle. Women who are overweight have a higher risk for developing breast cancer, as do women who practice unhealthy lifestyle habits, such as being sedentary, smoking, excessive alcohol consumption and consuming an unhealthy diet.
Genetics also take on a role in breast cancer risk. Up to 10 percent of breast cancer cases are believed to be linked to genetic mutations, which may be passed down from a parent.
BReast CAncer gene one (BRCA1) and BReast CAncer gene two (BRCA2) are actually genes that everyone has in their bodies. These genes carry out cellular repair for maintaining the health and function of the breasts as well as of the ovaries and other cells in the body. When either of these genes undergoes a mutation, they can no longer carry out their tasks as effectively. These ineffective genes get passed down through subsequent generations. Having one of these mutations does not seal a patient’s fate that they will develop breast cancer, but their risk does increase. It is important to remember that, while the incidence is much lower, men can also develop breast cancer, and they can develop the BRCA1 and BRCA2 mutations and pass them down to their offspring.
Just as knowing the risk factors for developing breast cancer is a crucial step toward early detection, being aware of the factors that contribute to the likelihood of carrying a genetic mutation is important. Women are more likely to have the BRCA1 and/or BRCA2 mutation(s) if:
Laboratory testing to detect the presence of these mutations should be considered for any female patient who falls into any of the above groups or carries any of the aforementioned risk factors of breast cancer. Blood tests can detect the presence of BRCA1 and BRCA2 mutations.
Positive test results confirm the presence of one of these mutations and thus place the patient in a significantly higher risk category for developing breast cancer.
Tumors release specific proteins into the bloodstream. These proteins are known as tumor markers, and blood tests to seek out the presence of these tumor markers enable pathologists to detect cancer. There are several tumor markers that are associated with breast cancer:
The normal reference ranges for these tumor marker tests are:
While tumor marker tests alone are inadequate screenings for the initial diagnosis of breast cancer, they can be valuable tests for determining the best course of treatment for a patient with breast cancer, for evaluating the efficacy of the treatment protocol and for monitoring a patient for breast cancer recurrence.
The American Cancer Society guidelines recommend that women who test positive for BRCA1 or BRCA2, or women who have any of the aforementioned risk factors for developing breast cancer, should undergo annual mammogram screenings beginning at age 30. In addition to mammography, ultrasound and/or magnetic resonance imaging of the breasts may be recommended for some women based upon their risk factors and on findings from physical examinations and laboratory tests. Women who are not considered high risk for developing breast cancer are advised to undergo annual mammogram screenings starting at age 40 to 45. All women should discuss their risk factors with their physicians to come up with the appropriate plans of preventative screenings that will provide the best chances for early detection, less aggressive treatment protocols and complete and lasting remission.
By Larry Fox
By Cat Troiano
In the United States alone, nearly 400,000 individuals are either currently living with leukemia or in remission, and more than 60,000 additional individuals are projected to be newly diagnosed with the disease during 2019. Although leukemia is most commonly diagnosed in adult patients over the age of 60, it is the most commonly diagnosed form of childhood cancer in patients under the age of 20. In fact, one out of every three cancer cases in children and teens is leukemia.
Leukemia is one form of blood cancer. Other examples of blood cancer include:
More specifically, leukemia is a form of cancer that affects the body’s tissues that are responsible for the production of blood cells, namely the marrow component in bone as well as the lymphatic system.
Leukemia typically affects the production of white blood cells, which are the group of cells responsible for boosting the immune system to fight off invading pathogens. The white blood cells are abnormally formed, and the number of leukocytes exceeds the normal level. When blasts, which are immature blood cells, are abnormal and multiply too rapidly, the disease is categorized as acute leukemia. These immature cells are unable to carry out normal cellular functions. Conversely, in the case of what is considered chronic leukemia, mature white blood cells multiply too quickly, but less rapidly than the replication of the immature cells in the acute scenario. Because they are mature cells, they are able to carry out some normal cellular functions for a short time. The abnormal white blood cells that replace healthy white blood cells are leukemia cells.
White blood cells are collectively known as leukocytes. There are five different types of leukocytes in the human body:
Neutrophils are the body’s initial responders to target and fight infection. With a lifespan of only hours, the body must produce approximately 100 billion neutrophils a day. Neutrophils account for roughly half of the body’s white blood cells.
Eosinophils, which account for up to five percent of the body’s white blood cells, are responsible for fighting invading pathogens, such as bacteria as well as parasitic infections. When an individual suffers from allergy symptoms, it is because their eosinophils mistakenly interpret allergens as pathogenic elements and are working overtime to combat them.
Basophils make up only one percent of the body’s white blood cells. Basophils contain histamine, which act as a vasodilator to promote blood flow to the body’s tissues. Heparin, which is an anticoagulant, is also found in basophils to balance out the clotting effect of platelets so that the blood doesn’t clot too rapidly. Basophils play a role in inflammation when the body launches an immune response, such as when an allergen prompts an asthma attack.
Lymphocytes are subdivided into two types, which are known as T-cells and B-cells. These two groups of cells work together to fight illnesses. The T-cells are the army that is responsible for destroying invading pathogens, and the B-cells are those responsible for producing antibodies to recognize and fight future threats of infection when the body is exposed to pathogens.
Monocytes are the cleanup crew of the immune system, targeting destroyed pathogens and dead cells to remove them from the body’s tissues. Monocytes make up between five and twelve percent of the body’s white blood cells, and they are the largest of these cells.
Lymphocytic leukemia affects the body’s lymphocytes, which are found in lymph, the fluid that circulates the lymphatic system from the body’s tissues through the lymph nodes to aid in removing toxins and impurities.
Myelogenous leukemia affects the myeloid cells, which are the cells that play a role in the bone marrow’s production of white blood cells as well as red blood cells, also known as erythrocytes, and platelets.
Leukemia, like many cancers, occurs in a number of different forms. The four most common types of leukemia are:
There are other types of leukemia, such as myelodysplastic syndrome, hairy cell leukemia, chronic myelomonocytic leukemia, large granular lymphocytic leukemia, myeloproliferative disorder, acute promyelocytic leukemia and juvenile myelomonocytic leukemia, but these are rarer forms of the disease.
Acute leukemias develop rapidly and the presentation of symptoms comes on soon after the onset of the disease. Chronic leukemias can take years to develop and for symptoms to present.
Leukemia occurs more frequently in men than in women, it is more common in Caucasian individuals than in African-Americans, and the risk for developing leukemia increases with advancing age.
Other definitive risk factors are still being determined. Some potential factors that may increase one’s risk for developing leukemia include:
Patients with leukemia are at increased risk for infections and anemia. Signs and symptoms of leukemia include the following:
A complete blood count with differential test should be ordered for any patient who presents with any of these symptoms and carries any of the potential risk factors.
A complete blood count (CBC) with differential takes an inventory of each of the body’s blood cells, including the different types of leukocytes. This test may be used to detect the presence of a blood disease, to confirm the presence of a suspected blood disease, and to monitor the progression of the patient’s disease and efficacy of the patient’s disease treatment protocol.
The normal reference range for the total number of white blood cells (WBCs) in an adult patient is between 4,500 and 10,000 cells per mcL. The normal reference range for each type of WBCs in adult patients is as follows:
• Neutrophils – 2.0–7.0×109/l (40–80%)
• Lymphocytes – 1.0–3.0×109/l (20–40%)
• Monocytes – 0.2–1.0×109/l (2–10%)
• Eosinophils – 0.02–0.5×109/l (1–6%)
• Basophils – 0.02–0.1×109/l (< 1–2%)
Abnormally high white blood cell counts are indicative of infection, inflammation or a condition such as leukemia.
The normal reference range for red blood cells (RBCs) is:
Abnormally low red blood cell counts are indicative of anemia.
Hemoglobin is the oxygen-carrying protein component in blood. The normal reference range for hemoglobin (Hg or Hgb) is:
Hematocrit represents the percentage of the blood’s erythrocyte component. The normal reference range for hematocrit (Hct) is:
Mean corpuscular volume (MCV) evaluates the average size of the blood’s erythrocytes. The normal reference range for MCV is 80 to 95 fl.
The normal reference range for the blood’s platelet count is 150,000 to 450,000 platelets per mcL
The normal reference ranges for infants, children and teens vary, depending on the gender and age of each patient.
Abnormally elevated leukocyte counts in a leukemia-suspect patient should prompt the ordering of additional diagnostic tests, which may include any of the following to confirm the diagnosis, to determine the type of leukemia and to evaluate the extent of which the leukemia has advanced:
As the disease advances, leukemia cells in the bloodstream accumulate in such organs as the liver, spleen, lymph nodes and other organs. Periodic comprehensive metabolic profiles should be ordered in conjunction with CBC with differential tests to monitor organ function, and additional diagnostic imaging tests, such as ultrasounds and magnetic resonance imaging, of any affected organs should also be considered.
The treatment plan and prognosis for a leukemia case depends on the patient’s age, which type of leukemia the patient has and how far along the disease has progressed. Treatment options include:
As research continues in an ongoing search for a cure, clinical trials for new treatment protocols may be available to qualifying patients. As with most health conditions, the earlier a diagnosis is made and treatment can be implemented, the higher the chances are for achieving remission, and early detection begins with laboratory testing.